There are multiple contamination control strategies (CCSs) that manufacturers use to provide a sterile/aseptic environment for formulating and filling sterile drug products. The three most commonly used systems are
- Cleanrooms
- RABS (Reduced Access Barrier Systems) units
- Isolators
This article will explain these three options and compare and contrast the strengths and weaknesses of each system.
Many modern pharmaceutical products are produced under aseptic (sterile) conditions. These products cannot be sterilized in their final dosage forms, because the sterilization process itself could have harmful effects on the product. For example, most biologically derived materials will be damaged or destroyed when subjected to sterilization conditions such as high heat or radiation. Since these products cannot be sterilized after the fact, the conditions of sterility must be designed into the manufacturing process. The environment in which the product is packaged is a critical component of that process.
Aseptic processing entails individually sterilizing each separate component that goes into the product, using appropriately validated methods, and then combining those now-sterile materials into the final dosage form under conditions that minimize or eliminate the potential for contamination from an outside source. Components of the final dosage form include:
- Containers (such as vials, syringes, injector cartridges, etc.)
- Closures (such as vial stoppers, syringe or injector plungers, etc.)
- Formulated drug product
- Any materials that come into contact with the product during the manufacturing process, including transfer lines, fill needles/nozzles, product filters, and buffer containers, are considered product-contact materials
Once sterilized, these components must be protected from the introduction of potential contaminants, most critically from potential infectious agents such as mold or bacteria. To maintain the sterility of these components, the environment that they are handled in must be strictly controlled. The methods listed above are the most widely used for providing a pristine environment.
I. Cleanrooms
The cleanroom has traditionally been the most widely used environment for aseptic manufacture. A cleanroom is primarily defined, or categorized, by the purity of the air in the room with respect to particulate matter of defined sizes. Air purification is typically done using High Efficiency Particulate Air (HEPA) filters to retain and remove particulate matter from the air.
In addition to use in pharmaceutical manufacturing, cleanrooms have traditionally been used in the manufacture of electronics (especially semiconductors and microelectronics, including chips), aerospace, optics and lasers, and other areas where contamination represents a threat to the proper manufacture or operation of the products.
According to the International Standards Organization (ISO)1, a cleanroom is
[a] room within which the number concentration of airborne particles is controlled and classified, and which is designed, constructed, and operated in a manner to control the introduction, generation, and retention of particles inside the room
Other cleanliness attributes, such as chemical, viable, or nanoscale concentrations in the air, or surface cleanliness, and/or other relevant parameters such as temperature, humidity, pressure, etc., may also be controlled in a cleanroom.
ISO lists specified classifications of cleanrooms ranging from ISO 1 (the lowest listed allowable levels of airborne particulates) to ISO 9 (the highest listed levels). Each classification has limits for the concentration (in counts/m³) of particles of specified sizes, ranging from 0.1 μm to 5 μm.
In addition to the specification in allowable particles, cleanrooms must meet additional criteria to be qualified for use in pharmaceutical manufacturing. The National Environmental Balancing Bureau (NEBB) lists the following requirements:
- The materials of construction (MoC) must be designed to meet requirements for ease of cleaning (e.g., non-porous materials) and resistance to cleaning agents (e.g., stainless steel or chemical-resistant polymers). The MoC must be non-shedding and non-organic to prevent the introduction of particles into the room.
- Cleanrooms must be kept at an elevated working pressure with respect to their surrounding environments. This is done to ensure the desired flow of air when the cleanroom is breached (e.g., when a door or pass-through is opened): air must always flow outward from cleaner environments to less clean, never in the reverse direction.
- Airflow in cleanrooms must be uniform and non-turbulent and within a defined range for velocity.
- The integrity of the HEPA filters must be confirmed periodically to ensure that there are no localized “hot spots” of potential high particulate contamination.
Operators working in cleanrooms have strict, well-defined requirements for gowning and behavior. They must be trained on how to properly gown to enter the cleanroom and how to behave while working in that environment. Full (i.e., 100% coverage) gowning is normally required. Behavioral restrictions include how to move (smoothly and without sudden, jerky motions) and where to position oneself and one’s body parts (e.g., head, arms, and hands). Operators usually face restrictions on the use of makeup and wearing of jewelry, may face restrictions on smoking or other behaviors even outside the cleanroom, and must maintain their health and hygiene in order to ensure that they are not posing a risk of contamination inside the cleanroom.
Cleanrooms have a long history of use in a variety of operations, and guidance and regulations on their operation are well characterized.
The primary benefits of cleanrooms are their relatively lower start-up costs and ease of qualification and use. Cleanrooms can be significantly easier and less expensive to install and qualify than the other contamination control strategies.
However, in the pharmaceutical industry, there is a perceived trend away from aseptic manufacturing in cleanrooms. The lack of true barriers between operators (the most significant potential for contamination by far) and the products they are working on means that true control is much harder to guarantee than with other strategies. Cleanrooms often utilize curtains to separate operators from the “critical zones” where product may be exposed (most prominently in the filling area itself). Operators are able to breach this separation with comparative ease.
Additionally, the long-term costs of operating cleanrooms may be higher than that for other contamination control strategies. In most cleanroom designs, there is not just one cleanroom but a series of increasingly more stringent (i.e., cleaner) cleanrooms leading from the area of no control to the critical areas where filling takes place. An operator may have to pass through multiple rooms or interlocks, with increasingly strict gowning and behavioral requirements, to access the critical areas. All of these areas, not just the critical zone, must be maintained and periodically qualified. For example, a typical pharma use has a filling area in an ISO Class 5 zone. The area surrounding this critical zone is normally classified as ISO Class 7 or better. If any zone is compromised, the continued operation of the entire line is threatened.
Although cleanrooms have a long history of successful use in the pharmaceutical manufacturing industry, it is likely that moving forward fewer and fewer new manufacturing operations using this technology will be commissioned, and existing lines will over time be upgraded or replaced as they approach the ends of their productive lifespans.
II. RABS
RABS stands for Restricted Access Barrier System. This is a technology best described as “in-between” the traditional cleanroom and a true isolator, and as such has costs and benefits that represent a middle ground between the other two strategies.
The primary benefit of a RABS when compared to a cleanroom is that the RABS does offer a true barrier between the operator and the critical filling areas. Instead of a curtain, the RABS utilizes a solid wall, typically of glass or chemically resistant polymer, separating the operator from the product. Access into the RABS during manufacturing is usually restricted to the use of sealed glove ports.
RABS typically include the following characteristics:
- Rigid wall enclosure to separate operators from the critical zone
- Unidirectional airflow through HEPA filters to provide at minimum ISO Class 5 quality air that flows in a single path (i.e., no recirculation) through and out of the RABS chamber
- Glove ports for operator interaction with the RABS interior
- Sterile transfer ports to allow entry of previously sterilized materials into the RABS interior
The same requirements for MoC, elevated differential pressure, non-turbulent airflow, and routine HEPA filter integrity verification that apply to cleanrooms are also in place for RABS units.
RABS are typically used in a surrounding environment of ISO Class 7 or better quality.
RABS may have access doors or panels that can be opened or removed during setup, but these are not typically used following sterilization of the RABS interior. If they are to be used during operation, there must be strict restrictions on how, when, and why they are opened.
RABS on average have higher startup costs than cleanrooms but are less expensive than isolators. Additionally, the timelines for construction, installation, and commissioning bridge the gap between cleanrooms (lower time lag) and true isolators (higher time lag). The gowning and behavioral restrictions on operators using RABS are less stringent than those for cleanrooms (provided that doors in the barriers, if present, remain closed following sterilization and during operation).
III. Isolators
Isolators represent the most stringent contamination control technologies currently in use in pharmaceutical manufacturing. An isolator is a fully contained environment that provides absolute separation between the critical filling areas and the surrounding environment, including operators.
Isolators are usually fully enclosed units, although some “open isolators” do exist. Isolators have their own air purification system built in, instead of relying on external air filtration. The interior of the isolator is maintained at positive pressure with respect to the outside environment, typically at a pressure of not less than 0.05 in H₂O. Access to the isolator interior is usually through closed glove ports (or half-suits for larger units) and specially designed transfer ports (such as rapid transfer ports, or RTPs), maintaining separation between the operator and the critical areas. Manipulation of the interior is frequently done using robotic or automated systems, rather than direct operator interaction.
Automated sterilization-in-place (SIP) of the interior of an isolator is standard. This allows the chamber and its contents to be sterilized in situ, without opening a door or otherwise breaching the containment.
Isolators can be used in surrounding environments that are less strictly controlled than other contamination technologies, as the isolator itself provides the sterility assurance needed for aseptic processing. ISO Class 8 or 7 environments are typically sufficient. Operators working with isolator systems face less-stringent gowning requirements as well, as they can only manipulate the interior of the isolator through sealed glove ports or automated (e.g., robotic) mechanisms.
Isolators are ideal for working with highly potent or potentially hazardous materials, as the isolated interior protects in both ways—the product is safeguarded against external contamination, and the operators in the surrounding area are protected against exposure to the materials inside.
Then start-up costs for isolators are the highest of the three contamination control strategies discussed. Additionally, changeover between different products may be more arduous. Isolators are best suited for single-product lines, or at least products that can be filled using the same equipment change parts and/or parameters.
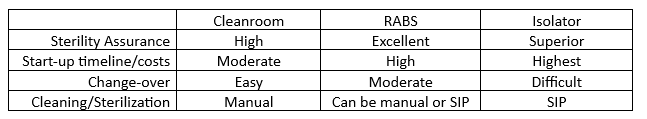
IV. Contrast
V CONCLUSION
The choice of what style of contamination control is utilized by the pharmaceutical manufacturer is a critical one. CCS technologies continue to advance, with improvements in all three styles continuing to emerge. Manufacturers must balance cost, commissioning timeline, and flexibility against the contamination risk to their projected product stream. No one method of CCS is perfect for all manufacturers. As manufacturing technologies continue to improve, the ability to produce medications with greater and greater levels of sterility assurance will continue to grow.
1 ISO 14644-1:1999 Cleanrooms and associate controlled environments – Part 1: Classification of air cleanliness by particle concentration
2 NEBB Procedural Standards for Certified Testing of Cleanrooms, Third Edition – October 2009
